Factors and solutions for acne development
Acne, not a life-threatening disease but certainly a life wrecking one and it can strike at any age. A genetic disease of the pilosebaceous unit, acne has often been considered a teenage problem; however, this skin concern extends well into adulthood and old age. Adult acne is more likely to develop in females than males due to hormonal influence and chronic stress; however, males do still suffer with breakouts and will need advice and support. Unlike teenage acne, which presents with lots of oil and comedones, the lesions in an adult’s skin tend to be more inflamed, persistent, and are more prone to hyperpigment.
When considering the best approach to dealing with the skin, therapists and medical practitioners alike focus on the development of this disease. There are four key factors that happen within acne pathogenesis:
1) Over proliferation of cells or hyperkeratosis. Keratinized cells are found in the Stratum Corneum; however, these cells line the sebaceous follicle resulting in about 4-5 times the amount of dead skin cells in an acneic skin. In an adult skin there is a deficiency of linoleic acid in the sebum, and this is believed to contribute to hyperkeratosis leading to comedones and the blocking of pores. Acneic skins also have less lamellar bodies in the Stratum Granulosum. These lamellar bodies initiate the desquamation process and therefore, a deficiency links to the cell proliferation.
2) An overproduction of sebum. There is an association between local overproduction of active androgens (testosterone) and acne. High testosterone levels have been implicated with enhanced sebaceous gland activity and studies have shown that acne patients produce higher rates of testosterone and dihydrotestosterone (DHT) in their skin. Sebaceous gland cells possess the necessary enzyme 5α-reductase that converts testosterone to dihydrotestosterone. When the potent androgen DHT binds to the nuclear androgen receptor (AR) on sebaceous gland cells, more sebum is produced.
3) Bacterial growth with Cutibacterium acnes (C. acnes) colonization. Cutibacterium acnes are the relatively slow growing, typically aerotolerant anaerobic, Gram-positive bacterium linked to acne. Although recognized as a part of the commensal flora of human skin, they can also act as an opportunistic pathogen in Acne Vulgaris. Contrary to what was previously thought, proliferation of C. acnes is not the trigger of acne, patients with acne do not harbour more C. acnes than other skins. Instead, the loss of the skin microbial diversity together with the activation of the innate immune system may lead to this chronic inflammatory condition instead.
4) Inflammation and the initiation of the immune response. The classic paradigm of acne is usually listed as the formation of micro-comedones from sebum and dead skin cell build up, and C. acnes colonization resulting in inflammation. Based upon recent studies, researchers are starting to investigate the possibility that inflammation actually precedes the formation of a comedone, and that inflammation exists in some form at every stage of acne pathogenesis including uninvolved follicles.
Inflammation may initiate the acne pathogenesis by stimulating pro-inflammatory cytokines such as Interleukin 1 (IL-1α, a comedogenic cytokine). These inflammatory cells have been reported to induce hyperkeratinisation in the follicle. Another hypothesis for the stimulation of IL-1α is the increase of sebum production and the decreased levels of linoleic acid. We also know that IL-1 plays a central role in the regulation of inflammatory and immune responses in general.
These new findings are groundbreaking as they may alter the way acne is approached by both aestheticians and medical staff. Imagine if by helping to reduce the inflammatory response in the skin either through product or ingredients or medication, or even a change in diet, the development of acne could be effectively slowed down.
It is important to be aware when approaching acne, that you are working within your scope of practice. When is it time to pass your client over to someone who can help? As therapists, we can support an acne sufferer by reducing the over-production of skin cells with exfoliation, we can use ingredients known to reduce sebum production or bacteria and we absolutely have the skills and ingredients to reduce inflammation. It is vital to successful outcomes; however, to acknowledge that we can’t “treat” acne and that we may need to pass our client over to a medical professional to support. This approach can be seen as a 360-degree approach as it works both ways. When does a medical practitioner recognize that the side effects of some well-known acne treatments such as irritation and chronic dryness can be supported by skin therapists. This approach can be seen as a revolving door between medical professionals and skin professionals to give clients and patients a strong 360-degree approach to helping them with their skins. Relationships built between industries is vital to achieving success especially as new ingredients and innovations occur frequently in both sectors.
One such development is the use of salicylic acid within the professional field. this beta-hydroxy acid has been used for many years in the reduction of skin lesions due to its keratolytic properties and ability to remove sebum plugs from the skin follicles. salicylic acid is also a phenomenal anti-inflammatory agent with anti-bacterial properties making a go to ingredient for many product companies.
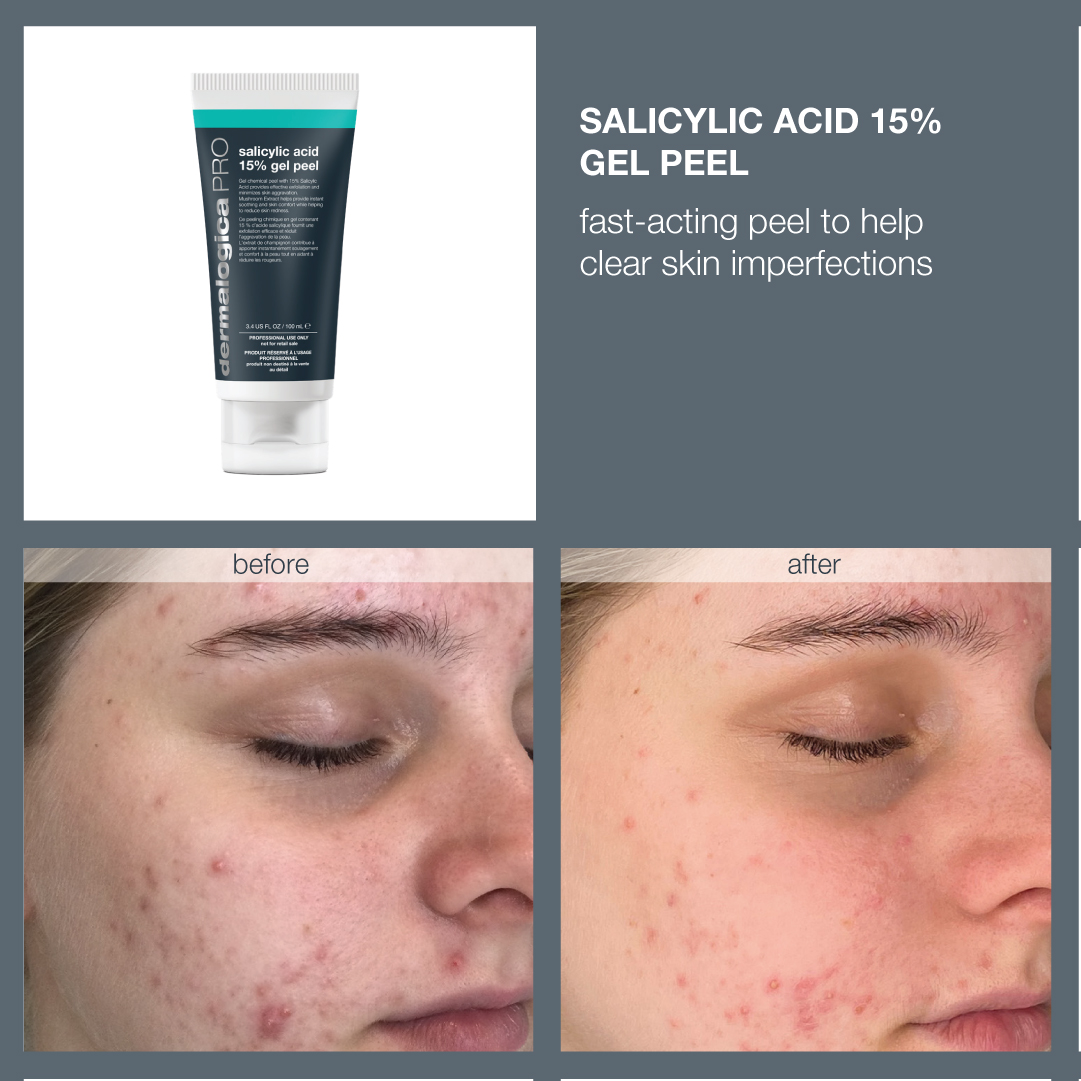
Dermalogica is excited to launch a new PRO innovation in the form of Salicylic acid 15% gel peel. This solution is unique in its approach and is designed to target not only the inflamed breakouts but also minimize skin discomfort due to the gel-like consistency. Salicylic acid 15% gel peel provides potent exfoliation combining the power of salicylic acid at a 15% strength alongside a plethora of other ingredients. Albatrellus mushroom protects the skin from stress and reduces inflammation, while white shiitake mushroom reduces inflammation and the melanin content within the skin reducing the post-inflammatory hyperpigmentation often associated with adult acne. This professional only peel is showing great signs of being a game changer in the skin care industry for 2023.

Sarah Hughes
Mediclinic training manager for IDI and Dermalogica



